Long title, I know. But there was a lot of news today! Here is a quick breakdown of some of the pieces that on the science side of things, stick out to me.
Oh, and this is your daily reminder that I am not a doctor or a medical professional. I didn’t go to college for this stuff, either. In fact, I don’t think I took a single medical-related course in college. But I am a scientist. And I am trained as a journalist, too. So, I put these together in hopes that I can track down useful information as a journalist and translate it into regular English as a scientist.
I’m not perfect, either. Some of this data may be “old news” to some of you. Other reports may be information you don’t necessarily care about.
But I’m just trying to act as a lens for all of the information that is bombaring all of us on a daily basis with this COVID-19 thing.
CDC & WHO Numbers
Total Worldwide Cases: 462,484
Total Worldwide Deaths: 20,834 ; 4.5% mortality rate
Total United States cases: 68,440
— Travel-related: 636
— Close contact: 1,074
— Under investigation: 66,730
Total deaths: 994 ; 1.4% mortality rate
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, and US Virgin Islands

Johns Hopkins Data
Total Worldwide Cases: 531,860
Total US cases: 85,653
Total US deaths: 1.290 ; 1.5% mortality rate
Total US recovered: 713
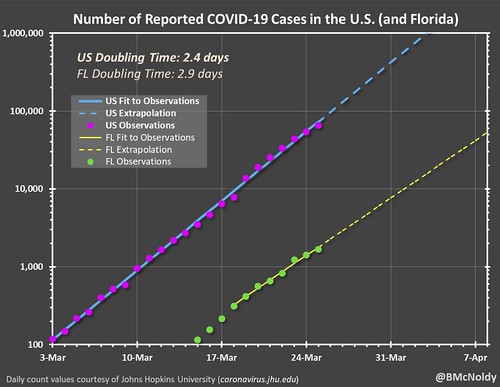
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put that chart together. As it notes, it is pulling numbers from the Johns Hopkins totals. It shows the double-time of cases as about two-and-a-half days.
Regional Statistics
| Total Cases | Total Tested | Deaths | Percent-positive | Mortality Rate | |
| Mississippi | 485 | 2776 | 6 | 17.47% | 1.24% |
| Louisiana | 2035 | 15775 | 83 | 12.90% | 4.08% |
| Alabama | 531 | 4082 | 1 | 13.01% | 0.19% |
| Tennessee | 957 | 14909 | 3 | 6.42% | 0.31% |
| Arkansas | 349 | 1882 | 3 | 18.54% | 0.86% |
| Total | 4357 | 39424 | 96 | 11.05% | 2.20% |

Note: There is no map available for Tennessee.
New Research
A press release from Mount Sinai mentioned that a “… team of researchers and clinicians in microbiology, virology, pathology, molecular science, and immunology at the Icahn School of Medicine at Mount Sinai (ISMMS) and The Mount Sinai Hospital (MSH) have been working together.. “to get an “end-to-end” testing, diagnosis, and treatment plan for people with COVID-19.
Mount Sinai is a hospital in New York, where the highest density of cases is currently in the United States.
The idea is that they would test to see if a patient is positive or negative. If positive, they would check to see what the “viral load” was in the test. That would determine, in essence, how infected the patient and what treatment options would be best. This would differ from the current means of testing which is just to determine if patients are positive or negative, and then if positive, sending them home to quarantine.
Also from Mount Sinai, researchers are working on figuring out if we can determine if people were once infected by COVID-19. And I’m going to paste in the piece from the hospital, but I don’t think I could explain it any better,
To help uncover just how widespread the novel coronavirus is within communities, a team led by virologist Florian Krammer, PhD, Professor of Microbiology at the Icahn School of Medicine at Mount Sinai, developed a serological enzyme-linked immunosorbent assay (ELISA) test. This test measures the presence or absence of antibodies to the virus in people’s blood. Similar to the most commonly used tests for other viruses, such as hepatitis B, this test shows whether a person’s immune system has ever come into contact with the virus (even months ago). There are three main advantages to this test: providing an accurate picture of how many people have been infected; identifying people with new immunity to SARS-CoV-2 who could care for COVID-19 patients at zero or minimal risk; and identifying newly recovered patients with high antibody levels who can donate their antibody-rich blood, known as convalescent plasma, to potentially save other patients with severe COVID-19. Initially the testing will be limited to potential plasma donors until testing capacity increases.
The team began working on this serological assay in January, before COVID-19 had been seen in the United States. To make this test, the researchers cloned animal cells to produce copies of the telltale “spike” protein that is present on the surface of SARS-CoV-2. That protein is highly immunogenic, meaning that people’s bodies see it and start making antibodies that can lock onto it. The test involves exposing a sample of blood to bits of the spike protein. If the test “lights up,” it means that person has the antibodies. Viviana Simon, MD, PhD, Professor of Microbiology at ISMMS, was instrumental in the design and implementation of the test, which has been approved for clinical use by the New York State Wadsworth Laboratory and is currently undergoing validation and urgent implementation. ISMMS medical students are establishing a social media campaign to identify volunteers to be tested.
“Our test can pick up the body’s response to infection as early as three days post-symptom onset and it could help locate survivors who are ‘hyper-immune,’” says Dr. Krammer. “Those people could then potentially donate their convalescent plasma to help very sick COVID-19 patients in intensive care units to help boost their immunity.”
The sensitive and specific identification of SARS-CoV-2 that ELISA provides will also support screening of health care workers to identify those who have already been exposed and are already immune. Those staff could then be deployed to the front lines to perform the riskiest tasks—like intubating a person infected with the virus—without worrying about getting infected or spreading the disease to colleagues, other patients, or their families. To learn the true extent of infections, the next step will be for researchers to carry out these serological surveys via blood draws from large numbers of people in an outbreak area, which may tell them exactly how many cases have gone unnoticed.
According to Dr. Krammer, efforts by the team at Mount Sinai and a few others developing similar tests (including the U.S. Centers for Disease Control and Prevention) to carry out a wider survey are just getting started, so it will likely be some time before scientists learn just how widespread SARS-CoV-2 is. The Mount Sinai Hospital Clinical Laboratories are also sharing specimens from recovered patients with the New York State Wadsworth Laboratory to assist other facilities in this effort.
This is new research, so like always, look at it with a skeptical eye until it has been peer reviewed. But it also means that our medical community is doing amazing things.
Another study, titled, “Potent human neutralizing antibodies elicited by SARS-CoV-2 infection” is in the process of further peer-review. This is pulled from Johns Hopkins:
A new preprint in BioRxiv describes a study that isolated and characterized a number of potential neutralizing antibodies for SARS-CoV-2. The studies results found that antibody response was specific to SARS-CoV-2 at specific binding domains, but that there was recognition of other coronavirus species in other unknown regions. The authors emphasized a need to explore the cross reactivity outside of noted binding sites but they expressed optimism that the findings show promise for new therapeutic and vaccine candidates.
Semi-related, but medical research papers have the some of the craziest graphics.

I’m not sure how to read that. And I think it is amazing that some people are smart enough to understand it.
A couple podcasts
Here is some great information on COVID-19 from a handful of short podcasts
Harvard Medical
Your feelings arise from a misaligned ratio of stress to resiliency. The more resilient you become the less stress you’ll feel. Dr. Greg Fricchione, director of the Benson-Henry Mind Body Institute at Massachusetts General Hospital, describes the tools and techniques for building resilience into your life during stressful times so we can better manage our anxieties.
Dr. Todd Ellerin is an infectious diseases physician at South Shore Health in Weymouth Massachusetts, and an instructor in medicine at Harvard Medical School. He also serves as an associate physician at Boston’s prestigious Brigham and Women’s Hospital. He offers insight—and practical information– from the front lines in the battle to stem COVID-19.
Mayo Clinic
Each day, the Mayo Clinic Q&A podcast shares the latest information on the COVID-19 pandemic. On today’s episode, Dr. Gregory Poland, an infectious diseases expert and head of Mayo Clinic’s Vaccine Research Group, answers listeners’ coronavirus questions.
Mount Sinai
Brendan Carr, MD, Chair of Emergency Medicine for the Mount Sinai Health System, had been at his job for less than a month when the first COVID-19 patient in New York City was diagnosed. Now he finds himself at the center of the largest coronavirus outbreak in the United States. With new patients flooding the city’s emergency rooms, Dr. Carr races to make sure his doctors and nurses have everything they need–from staff to ventilators. In this interview, he talks about the tough decisions he’s facing, and how he’s coping with enormous pressure to save lives.
Annals On-Call
Dr. Centor discusses the epidemiology of the novel coronavirus responsible for COVID-19 with Dr. David Fisman of the University of Toronto. (From March 10th)
A quick note about the EPA
There was a TON of information flying around today about the EPA loosening restrictions amid the COVID-19 outbreak. Many people found this to be a strange time to relax regulations that keep the environment safe given humans need a clean environment (air & water) to survive.
Now, I will claim no expertise in “reading between the lines” of press releases from Government entities, but here is what a piece of the press release said:
EPA’s temporary enforcement discretion policy applies to civil violations during the COVID-19 outbreak. The policy addresses different categories of noncompliance differently. For example, under the policy EPA does not expect to seek penalties for noncompliance with routine monitoring and reporting obligations that are the result of the COVID-19 pandemic but does expect operators of public water systems to continue to ensure the safety of our drinking water supplies. The policy also describes the steps that regulated facilities should take to qualify for enforcement discretion.
“EPA is committed to protecting human health and the environment, but recognizes challenges resulting from efforts to protect workers and the public from COVID-19 may directly impact the ability of regulated facilities to meet all federal regulatory requirements,” said EPA Administrator Andrew Wheeler. “This temporary policy is designed to provide enforcement discretion under the current, extraordinary conditions, while ensuring facility operations continue to protect human health and the environment.”
The temporary policy makes it clear that EPA expects regulated facilities to comply with regulatory requirements, where reasonably practicable, and to return to compliance as quickly as possible. To be eligible for enforcement discretion, the policy also requires facilities to document decisions made to prevent or mitigate noncompliance and demonstrate how the noncompliance was caused by the COVID-19 pandemic.
This policy does not provide leniency for intentional criminal violations of law.
The policy does not apply to activities that are carried out under Superfund and RCRA Corrective Action enforcement instruments. EPA will address these matters in separate communications.
Again, I’m no expert at reading between lines, but this doesn’t appear to be as dire a situation as some were attempting to make it. It seems to me like the EPA is recognizing that certain facilities tasked with “monitoring” are often run by humans, and with the pandemic those humans may not be able to actively monitor things. And without active monitoring there is a chance some facilities may go into non-compliance. And the EPA understands this and is willing to offer leniency for a short period of time so long as those facilities document reasons for non-compliance and the decisions that led to it.
To me, on paper, this seems reasonable given the circumstances. That said, how it is enforced will be another matter. One which may become as muddied as the waters the EPA is tasked with protecting. Only time will tell.
Letter from the Editor
I know a lot of us are getting “News Fatigue” with this Coronavirus stuff. And we want life to go back to the way it was before all of this started. Personally, I miss baseball. And I know some people still feel like it is being blown out of proportion. And that’s fine. I’m not here to tell you how to think or feel – except about one thing.
We need to look out for others. Right now, especially.
And especially those who are older since this virus disproportionately affects those who are older than 60. Of the five deaths in Mississippi from this virus, all of them were older. So, we need to do what we can to help those people stay informed so they can avoid becoming sick. When was the last time you called a grandparent, an uncle, a former teacher, a neighbor, or someone else you know that is older than 60?
Do me a favor. Give them a call today. Ask them how they are doing. Make sure they are getting good information about all of this.
Then, if you could, avoid being out in public and practice good social distancing to help slow the spread of the virus, too.
I made a post a few weeks ago when a high-ranking government official touted the “good news” that only older people were dying. Now other government officials are claiming those older people would be happy to die from this virus.
That is a very weird turn-a-phrase way of trying to claim certain people are expendable. And no living, breathing human is expendable. No matter what. I said it before and I’ll say it again: Older people matter. We have *got* to realize this.
And they matter for, like, infinity reasons. I wouldn’t even know where to begin to list them all.
And right now in order to protect them – and others, this virus infects everyone! – we all need to make changes to our daily lives for a while in order to make sure those people are going to survive. Literally. Because life will go on. But if we don’t make these changes, for some, it will kill them. Literally.
And I don’t think any of us want that to happen.
Before you go, a quick note on proper nomenclature
The World Health Organization, likely in an attempt to combat misinformation, posted a quick note on the naming of the coronavirus disease (COVID-19) and the virus that causes it.
Official names have been announced for the virus responsible for COVID-19 (previously known as “2019 novel coronavirus”) and the disease it causes. The official names are:
Disease: coronavirus disease (COVID-19)
Virus: severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
WHO has begun referring to the virus as “the virus responsible for COVID-19” or “the COVID-19 virus” when communicating with the public. Neither of these designations are intended as replacements for the official name of the virus as agreed by the ICTV.
That is it. Just those two names. That is why I have also started (trying my best) to use the same terminology as the WHO. To combat misinformation.

