I’m still not a doctor, but I do want to help everyone get a better handle on the pandemic.
Latest Numbers
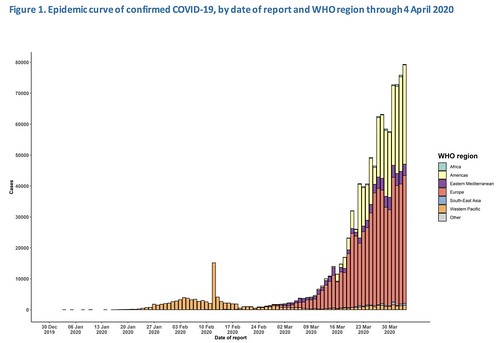
WHO Numbers
Total Worldwide Cases: 1,051,635
Total Worldwide Deaths: 56,985
CDC Numbers
Total United States cases: 277,205
— Travel-related: 1,388
— Close contact: 4,325
— Under investigation: 233,566
Total deaths: 6,593
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, the Northern Mariana Islands, and the U.S. Virgin Islands
COVID-19 cases reported by other medical sites:
Johns Hopkins
Total Worldwide Cases: 1,202,236
Total Worldwide Deaths: 64,753
Total Worldwide Recovered: 246,457
Total US cases: 311,554
Total US deaths: 8,488
Total US recovered: 14,786
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put a chart together of the growth. As it notes, it is pulling numbers from the Johns Hopkins totals.
Regional Numbers
| Cases | Tested | Deaths | Percent-positive | Mortality Rate | |
| MS | 1455 | N/A | 35 | #VALUE! | 2.41% |
| LA | 12496 | 54304 | 409 | 23.01% | 3.27% |
| AL | 1633 | 10847 | 44 | 15.05% | 2.69% |
| TN | 3321 | 41391 | 43 | 8.02% | 1.29% |
| AR | 743 | 10370 | 14 | 7.16% | 1.88% |
| Total | 19648 | 116912 | 545 | 16.81% | 2.77% |
A few states in the region do release the number of hospitalized people due to COVID-19. Those numbers are as follows:
Mississippi: 284
Louisiana: 1,726 (571 on ventilators)
Alabama: 212
Tennessee: 311
Arkansas: Not given
Making Estimates from past research
I talked about research from the Cruise Ships that may be relevant to estimating the number of cases without testing everyone (since that isn’t a feasible option). Plus, this type of estimate would make a good “first guess” at the number of asymptomatic people (the people who don’t feel sick, but are still infected), too.
This type of estimating isn’t perfect. In fact, it is far from it. And it is just an estimate. But based on the past research, it is at least a start.
| Estimated Symptomatic | Estimated Asymptomatic | Estimated total | |
| MS | 2219 | 487 | 2706 |
| LA | 19059 | 4184 | 23243 |
| AL | 2491 | 547 | 3037 |
| TN | 5065 | 1112 | 6177 |
| AR | 1133 | 249 | 1382 |
| Total | 29967 | 6578 | 36545 |
Numbers in perspective
I wanted to take a quick moment to look back a few weeks. Since I’ve started covering this pandemic, a lot has changed. I started doing these updates back in February in order to simply keep people “in the loop” with some the latest information from official sources and new information from the medical community.
Slowly they have morphed into a collection of numbers, guidance, tips, coping strategies, and a repository of medical research on COVID-19. And it has all happened so fast that I don’t think many of us (myself included) have stopped to realize just how fast the information is stacking.
On March 4th, my update on the latest numbers:
The latest available data on the CDC website shows:
– 60 total cases
– 6 deaths
– 12 states reporting Coronavirus
Today?
– 277,205 total cases
– 6,593 deaths
– 50 states, District of Columbia, Puerto Rico, Guam, Northern Marianas, and US Virgin Islands reporting cases
That is a – roughly – 450,000-percent increase in cases and about a 100,000-percent increase in deaths.
That is painfully sobering.
The jump is even incredible in just the last two weeks. Two weeks ago, on March 21st, I posted:
Total United States cases: 15,219 as of Friday (7.038 on March 19th)
— Travel-related: 337 (269 on March 19th)
— Close contact: 321 (276 on March 19th)
— Under investigation: 15,219 (6,493 on March 19th) – this number reflects the increase in testing.
Total deaths: 201 (97 on March 19th)
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, and US Virgin Islands
Today, that same breakdown looks like this:
Total United States Cases: 277,205
– Travel-related: 1,388
– Close contract: 4,325
– Under Investigation: 233,566
Total deaths: 6,593
It took from March 4th until the 21st, 17 days, to go from 6 to 201 deaths. It took from March 21st through April 4th, 14 days, to go from 201 to 6.593 deaths.
Since April 1st, in just three days, 1477 deaths.
Look, I’m not going to tell you how to feel. If you read these numbers and still think, ‘yeah, well more people die from the flu’ that is your right. But I will say Hurricane Katrina killed 1877 people, and I don’t recall people saying it was “no big deal” because the flu kills more people.
A timeline of research
This is not a comprehensive timeline by any means, and if you are curious about if something has been covered on this site with respect to COVID-19, I’ve set up this special Google Box to search this site for any topic:
March 4th
This was one of the first days the World Health Organization raised concerned about PPE.
WHO is getting concerned about another aspect of the Coronavirus – healthcare workers safety. Healthcare workers – nurses, doctors, etc – rely on things called personal protective equipment (PPE) to keep themselves in good health while surrounded by sick patients.
This helps protect the healthcare workers, and the people who come into contact with the healthcare workers.
March 11th
We found out that the incubation period lasted – on average – five days.
In a new research paper titled, “The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application” researchers from Johns Hopkins identified that the incubation period for Coronavirus is about five days.
The results of the research found that 5.1 days was the average time of incubation and around 97-percent of those who develop symptoms will do so within about 11 days. On top of that, researchers noted that only 101 out of every 10 000 cases will develop symptoms after 14 days.
March 13th
This was the day that the World Health Organization released information that dogs cannot transmit the virus.
Right now, the medical research community thinks – like SARS – it started in bats and, perhaps, civets. But there was a paper that noted that other animals could be transmitters – but only if infected by another animal.
Yushun Wan, Jian Shang, Rachel Graham, Ralph S. Baric, and Fang Li wrote in the Journal of Virology:
Pigs, ferrets, cats and non-human primates contain largely favorable 2019-nCoV-contacting residues in their ACE2, and hence may serve as animal models or intermediate hosts for 2019-nCoV
March 16th
We learned from a Doctor that:
In short, Sinclair says that, “..in lung, CoV2 prevents cells from making biological detergents to keep lung passages open. Acute respiratory distress follows. O2 levels fall” and “CoV genes 1 & 8 are predicted to interfere with heme, the red compound in blood, by kicking out the iron.” meaning “diabetics and elderly are more susceptible. Blood sugar levels usually increase as we get older, increasing the amount of glycated hemoglobin” thus “it destroys the lung so patients can’t take up oxygen AND reduces the body’s ability to carry oxygen.”
It was also the first time I heard about “long-term lung damage” from COVID-19:
Dr Owen Tsang Tak-yin, medical director of the authority’s Infectious Disease Centre at Princess Margaret Hospital in Kwai Chung, said doctors had already seen around a dozen discharged patients in follow-up appointments. Two to three were unable to do things as they had in the past.
“They gasp if they walk a bit more quickly,” Tsang told a media briefing on Thursday. “Some patients might have around a drop of 20 to 30 per cent in lung function [after recovery].”
March 19th
The National Institute of Health reported that a new paper published in the New England Journal of Medicine shows the Coronavirus can survive on surfaces for longer than originally anticipated.
The virus that causes coronavirus disease 2019 (COVID-19) is stable for several hours to days in aerosols and on surfaces, according to a new study from National Institutes of Health, CDC, UCLA and Princeton University scientists in The New England Journal of Medicine. The scientists found that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detectable in aerosols for up to three hours, up to four hours on copper, up to 24 hours on cardboard and up to two to three days on plastic and stainless steel.
It was also noted that:
The take-away from that is that four independentn cases in a population show a 50-50 chance it will become established. That may feel scary. However, the researchers also found that once restrictions were in place – and followed – it trimmed the transmission rate down to below the regular flu.
But the restrictions – self isolation, social distancing, etc – are pretty strict. And it remains to be seen if the United States will implement such restrictions.
Also, I made an extrapolation about the number of infected and deaths by the end of March. The numbers were off by a few days, but, sadly, still hold.
With a two-percent fatality rate of those 307,200 estimated people, 6,144 would die. And those who would die, would within six weeks as the virus took its course..
And while I have discussed the dangers of extrapolation before, and while this is an exaggerated example, this is why social distancing is so important. It will help curb those numbers dramatically if we all do our part.
March 22nd
We learned that someone – in this case a child – was asymptomatic and tested negative with the swab, but had the virus and was capable of spreading it to others.
A child in China who was diagnosed with the virus never became symptomatic. In a paper titled, “Detection of Novel Coronavirus by RT-PCR in Stool Specimen from Asymptomatic Child, China” the authors highlight that despite being asymptomatic, the virus was actually detected in stool samples. they wrote: “We report an asymptomatic child who was positive for a 2019 novel coronavirus by reverse transcription PCR in a stool specimen 17 days after the last virus exposure. The child was virus positive in stool specimens for at least an additional 9 days. Respiratory tract specimens were negative by reverse transcription PCR.”
March 24th
Harvard Medical released a report suggesting that people could be contagious before they show symptoms and long after they feel better
Research shows that people are possibly most contagious early in the course of their illness, when they are beginning to experience symptoms. Also, researchers have detected viral genetic material in patients several weeks after they’ve recovered. Harvard notes that “the significance of these findings is not fully understood,” but they do say that it is possible people may continue to be contagious for weeks after they are feeling better. Weeks.
March 25th
A new research paper that is due out in June, that is not-yet-peer-reviewed, titled “Estimating Risk for Death from 2019 Novel Coronavirus Disease, China, January–February 2020” that looks into the mortality rate in China. The numbers they looked through led them to conclude:
… the risk for death from COVID-19 in China as of February 11, 2020, were as high as 12% in the epicenter of the epidemic and as low as ≈1% in the less severely affected areas in China. Because the risk for death from COVID-19 is probably associated with a breakdown of the healthcare system in the absence of pharmaceutical interventions (i.e., vaccination and antiviral drugs), enhanced public health interventions (including social distancing measures, quarantine, enhanced infection control in healthcare settings, and movement restrictions), as well as enhanced hygienic measures in the general population and an increase in healthcare system capacity, should be implemented to rapidly contain the epidemic.
This was also, as best I can recall, the date I first reported about asymptomatic transmission showing up in research articles.
March 27th
Mount Sinai claimed to have found an effective way to treat patients
The Mount Sinai Health System claims that the researchers and doctors there plan to initiate a “plasmapheresis,” where the antibodies from someone who has recovered from COVID-19 will be transferred into critically ill person still fighting the disease. The hope is that the antibodies from the healthy person’s plasma will help fight off COVID-19 and neutralize it.
March 28th
I started offering first-hand accounts of the medical professionals working through this pandemic.
“I had to take time away from work for about 1.5 weeks, Seely said. “I had a coworker and close friend who had [COVID-19] with textbook symptoms. She was so spot on that they didn’t want to test her and waste a test, since tests were so far and few between at the time. I came down with symptoms about five days after she presented with symptoms. They wouldn’t test me either since they had to save tests for people needing to be admitted to the hospital. By the time they were able to test me, almost all of my symptoms were gone. The test came back negative. So unknown if I actually had it.”
March 31st
Smokers were added to the group of “high risk” individuals for COVID-19
According to the Mayo Clinic’s Dr. Gregory Poland of the Vaccine Research Group, people with lung disease or smokers “tend to be at higher risk for more severe symptoms from COVID-19.”
Serious symptoms could mean the development of pneumonia (an infection that inflames the air sacs in the lungs) and that may require hospitalization, the use of a breathing machine, or ventilator. As Dr. Poland points out, in some cases, “breathing difficulty coupled with pneumonia makes COVID-19 life-threatening.”
April 1st
The CDC published a report about asymptomatic transmission
The CDC published a report from Wycliffe E. Wei, MPH1; Zongbin Li, MBBS1; Calvin J. Chiew, MPH1; Sarah E. Yong, MMed; Matthias P. Toh, MMed,; Vernon J. Lee, PhD1, titled, “Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020” that looks at how people are passing the virus to others before they even know they have it.
Cluster A. A woman aged 55 years (patient A1) and a man aged 56 years (patient A2) were tourists from Wuhan, China, who arrived in Singapore on January 19. They visited a local church the same day and had symptom onset on January 22 (patient A1) and January 24 (patient A2). Three other persons, a man aged 53 years (patient A3), a woman aged 39 years (patient A4), and a woman aged 52 years (patient A5) attended the same church that day and subsequently developed symptoms on January 23, January 30, and February 3, respectively. Patient A5 occupied the same seat in the church that patients A1 and A2 had occupied earlier that day (captured by closed-circuit camera) (5). Investigations of other attendees did not reveal any other symptomatic persons who attended the church that day.
April 2nd
The University of Pittsburgh claims to have a vaccine for COVID-19.
UPMC and University of Pittsburgh School of Medicine scientists announced a potential vaccine against SARS-CoV-2, the new coronavirus causing the COVID-19 pandemic. When tested in mice, the vaccine, delivered through a fingertip-sized patch, produces antibodies specific to SARS-CoV-2 at quantities thought to be sufficient for neutralizing the virus.
The paper appeared in EBioMedicine, which is published by The Lancet, and is the first study to be published after critique from fellow scientists at outside institutions that describes a candidate vaccine for COVID-19. The researchers were able to act quickly because they had already laid the groundwork during earlier coronavirus epidemics.
Going Forward
On the research side of things, it looks like there is some promising new research with vaccines and treatments. The medical community is doing a fantastic job attacking this problem from – seemingly – every angle. Between researchers, doctors in hospitals, and retired medical professionals, everyone is chipping in.
For the rest of us, our job is simple: Avoid others. Whether we “feel fine” or not. Because, right now, for every next person we don’t get within-six-feet-of, we save the medical community another person potentially needing care.
So sit around the house! Be lazy! Watch a movie! Read a book! Do some gardening? Maybe call up an old friend or a favorite relative.
Just stay home. Because that is how we can all help right now.