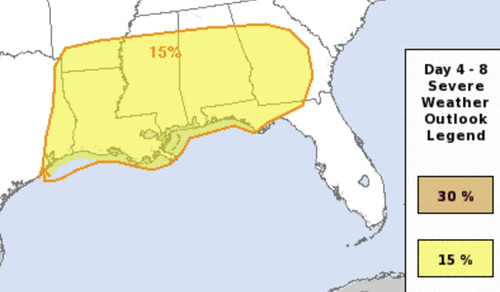
So, with severe weather on the horizon, I can’t burn this candle at both ends every day. Something has to give. And since my responsibility to keep you guys safe from severe weather comes first, these updates will likely be a bit “light” in the coming days as I spend more time working through the forecast data to make sure everyone is prepared for the potential for severe weather on Easter.
And, oh by the way, there is a potential for severe weather on Easter if you live in Louisiana, Arkansas, Mississippi, Alabama Florida and Georgia.
A brief reminder, too, that I am not a doctor. Nor a medical professional. I’m just a scientist that wants to help the world out by sharing information about this pandemic.
Latest Numbers
WHO Numbers
Total Worldwide Cases: 1,353,361
Total Worldwide Deaths: 79,235
CDC Numbers
Total United States cases: 395,011
— Travel-related: 1,864
— Close contact: 8,203
— Under investigation: 384,944
Total deaths: 12,754
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, the Northern Mariana Islands, and the U.S. Virgin Islands
COVID-19 cases reported by other medical sites:
Johns Hopkins
Total Worldwide Cases: 1,514,866
Total Worldwide Deaths: 88,444
Total Worldwide Recovered: 329,492 (a 29,000 person increase in one day!)
Total US cases: 431,838
Total US deaths: 14,768
Total US recovered: 23,865
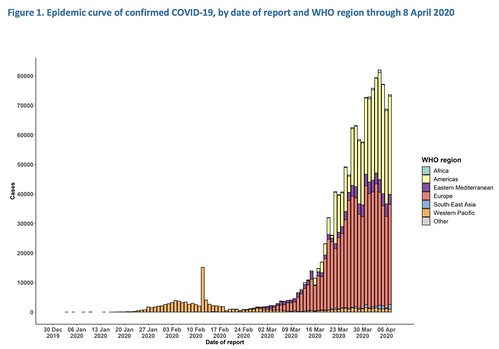
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put a chart together of the growth. As it notes, it is pulling numbers from the Johns Hopkins totals.
Regional Numbers
| Cases | Tested | Deaths | %-positive | Mortality Rate | |
| MS | 2003 | 20370 | 67 | 9.83% | 3.34% |
| LA | 17030 | 76640 | 652 | 22.22% | 3.83% |
| AL | 2499 | 18982 | 67 | 13.17% | 2.68% |
| TN | 4362 | 56618 | 79 | 7.70% | 1.81% |
| AR | 1077 | 14909 | 18 | 7.22% | 1.67% |
| Total | 26971 | 187519 | 883 | 14.38% | 3.27% |
A few states in the region do release the number of hospitalized people due to COVID-19. Those numbers are as follows:
Mississippi: 410
Louisiana: 1,983 (490 on ventilators) <- both numbers are down since yesterday
Alabama: 314
Tennessee: 449
Arkansas: Not given
Making Estimates from past research
I talked about research from the Cruise Ships that may be relevant to estimating the number of cases without testing everyone (since that isn’t a feasible option). Plus, this type of estimate would make a good “first guess” at the number of asymptomatic people (the people who don’t feel sick, but are still infected), too.
This type of estimating isn’t perfect. In fact, it is far from it. And it is just an estimate. But based on the past research, it is at least a start.
| Estimated Symptomatic | Estimated Asymptomatic | Estimated total | |
| MS | 3055 | 671 | 3726 |
| LA | 25974 | 5702 | 31676 |
| AL | 3811 | 837 | 4648 |
| TN | 6653 | 1460 | 8113 |
| AR | 1643 | 361 | 2003 |
| Total | 41136 | 9030 | 50166 |
What the new model data really means
The new pandemic model data from covid19.healthdata.org is out showing fewer deaths across the United States as schools remain closed, businesses limit customers, and people continue to practice Social Distancing.
So, what does that mean? Were the original numbers wrong? Are these numbers right? Why does it keep changing?
Think of it like weather, in a way. For those of you who watch my forecasts occasionally, I always say: “Leading up to an event, we know more as every day passes and as new data gets into the model. Every hour closer, there is more data available, and we know more about what will happen.”
This is very similar. The pandemic model is taking in new data (humans are now social distancing, humans are washing hands even more, treatments are being tried, researchers are finding new info) and the model produces a new forecast.
That doesn’t mean the old forecast was “wrong” but rather, the model didn’t have the same data in it that the model does now.
Just like weather models. Think about hurricane season. We always talk about getting the Hurricane Hunters into the storm to get back the data so we can put it in the models and get a much better idea about what was going to happen.
After we do that, we don’t say the previous forecast was “wrong” we simply say this new forecast is “better.”
So, if you hear anyone saying, “The experts were wrong about the number of deaths! They lied! Look at how they are changing things!” I would encourage you to stop them and explain that, just like predicting the weather, when the data changes, the models change.
And people running the models and producing the forecasts are doing the best they can to offer an accurate forecast with the data that is available.
And the new data shows that people are doing the right thing. And thus the numbers are coming down.
Infants and COVID-19
The CDC posted a new report, “Coronavirus Disease 2019 in Children — United States, February 12–April 2, 2020” that cites a couple of different studies about kids and COVID-19. There are a lot of numbers in here, but I needed to post the whole thing to give the last part some context.
Among 149,082 U.S. cases of COVID-19 reported as of April 2, 2020, for which age was known, 2,572 (1.7%) occurred in patients aged <18 years. In comparison, persons aged <18 years account for 22% of the U.S. population (3). Although infants <1 year accounted for 15% of pediatric COVID-19 cases, they remain underrepresented among COVID-19 cases in patients of all ages (393 of 149,082; 0.27%) compared with the percentage of the U.S. population aged <1 year (1.2%) (3). Relatively few pediatric COVID-19 cases were hospitalized (5.7%–20%; including 0.58%–2.0% admitted to an ICU), consistent with previous reports that COVID-19 illness often might have a mild course among younger patients (4,5). Hospitalization was most common among pediatric patients aged <1 year and those with underlying conditions. In addition, 73% of children for whom symptom information was known reported the characteristic COVID-19 signs and symptoms of fever, cough, or shortness of breath.
These findings are largely consistent with a report on pediatric COVID-19 patients aged <16 years in China, which found that only 41.5% of pediatric patients had fever, 48.5% had cough, and 1.8% were admitted to an ICU (4). A second report suggested that although pediatric COVID-19 patients infrequently have severe outcomes, the infection might be more severe among infants (5). In the current analysis, 59 of 147 pediatric hospitalizations, including five of 15 pediatric ICU admissions, were among children aged <1 year; however, most reported U.S. cases in infants had unknown hospitalization status.
The report they cite about the infection being more potent for infants is a study titled, “Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China,” and published in the Official Journal of American Pediatrics.
In that study, the researchers noted:
Recent evidence indicates that ACE2 is also likely the cell receptor of 2019-nCoV.20,21 It is speculated that children were less sensitive to 2019-nCoV because the maturity and function (eg, binding ability) of ACE2 in children may be lower than in adults.22 Additionally, children often experience respiratory infections (eg, respiratory syncytial virus [RSV]) in winter and may have higher levels of antibody against virus than adults.
Furthermore, children’s immune systems are still developing and may respond to pathogens differently from adult immune systems. However, we found that the proportion of severe and critical cases was 10.6%, 7.3%, 4.2%, 4.1%, and 3.0% for the age groups <1, 1 to 5, 6 to 10, 11 to 15, and >15 years, respectively. These results suggest that young children, particularly infants, were vulnerable to 2019-nCoV infection. Therefore, the mechanisms for the difference in clinical manifestations between children and adults remains to be determined.
There are a few new hypothesis in there that are likely to be researched in the coming months and years about why adults are more susceptible to severe infection than kids. But back to infants: One study I was reading – forgive me for not recalling the name of it – did also mention that younger children were more likely to be admitted to the hospital with COVID-19 symptoms. However, the authors of that study hypothesized that it may be a case that parents were more likely to seek medical care for younger children.
In short, when your kid is 12 and has a high fever and a cough, you tell them to relax, have some soup, and you care for them at home. When the child is much younger, parents may be more apt to bring the kid to a hospital with the same symptoms.
But that was just a hypothesis. There is still a lot of science left to do with all of this.
<h2
Johns Hopkins reports that among some countries dealing with this pandemic that under-reporting of deaths may begin – or has already begun – to occur. That would lead to an “underestimating” of the scale and severity of the pandemic.
We have previously reported challenges associated with reporting COVID-19 cases, in particular due to limited testing and a focus on the most severe cases. It has largely been assumed, however, that surveillance systems were accurately capturing COVID-19 deaths due to severe cases seeking care. Reports are emerging from around the world—including China , Ecuador , the United Kingdom , and the United States —that many potential COVID-19 patients may be dying without a proper diagnosis. In some cases, testing may not be available to test suspected cases after they die, and in others, patients may not be able to seek care due to overwhelmed local health systems.
Johns Hopkins reports that in many countries, patients die at home without seeking medical care nor testing. And, Johns Hopkins says, many of those victims may not be accounted for in the COVID-19 surveillance data.
Lesser discussed COVID symptoms
You may recall a brief report I posted a few weeks ago about a child in China that had the virus but was asymptomatic. They ended up finding out he had the infection, not by a swab, but from a stool sample.
Turns out, new data are coming to light explaining that may not be as uncommon. In this Q&A, Dr. Sahil Khanna, a Mayo Clinic gastroenterologist, answers questions about gastrointestinal (GI) symptoms related to COVID-19.
Note that while he says things are uncertain about transmission via stool material, he also says “I think we should assume that if there is somebody who has COVID-19, their stool, just like there respiratory sections, are potentially transmittable and are potentially infectious.”
A lot of people are recovering
More than 29,000 people recovered across the world since yesterday. That is some good news and a good place to end this post. Keep practicing social distancing and keeping helping others when you can, where you can. We are all human and we are all in this together.
And we will all get through this together, too.
All we have to do is practice social distancing. Good social distancing, too. Just because the “rule” says no gathering of 10 or more, doesn’t mean you should invite eight friends over. Do your best to isolate yourself and encourage others to do the same. Use technology to keep in contact with others, but keep physical distance.
And for those of you reading this in Louisiana and Mississippi… I know a lot of you made it through the worst of Katrina. And if you can make it through Katrina, you can make it through this. I believe in you.
Keep your head up, friends!