Y’all. You know me as someone who is straight-forward and transparent. I try to be sympathetic and empathetic to everyone’s situation. At all times.
A lot to unpack
Please know, I get it.
When I write, “I get it” I mean that I understand that all of this can feel overwhelming to a lot of you. The consequences of our actions today would have dire outcomes tomorrow. And the responsibility of that probably feels like anvils on your shoulders. I know how tough it can feel to choose to educate yourself on all of this. Daily. Hourly, even.
I get it.
As the chips really begin to fall in the coming days. And it feels like the world is coming to a stop, please know that we are all still here for each other. In America, we help those in need. We don’t leave anyone behind. And, if I may, I would encourage you to contact your neighbors to make sure they’re doing well. Then find send a message to someone, maybe at random, that you haven’t spoken with in a while. Check on them.
And if someone reaches out to you in the coming days, weeks, and months…. and you need help, ask. Don’t feel like it is a shot art your pride. Please try to avoid being too stubborn.
These are extreme times. And it is okay to admit that you can’t go at it alone. Because we all are going to need someone else at some point. Every. Single. One of us.
That is okay.
Because in America, we help those in need.
The numbers
I am not a medical doctor. I know a few, and they are all awesome! But I am not one. Nor am I a healthcare professional of any kind.
These updates are my way of helping everyone sift through the riff-raff. There is a lot of misinformation floating around. My goal with these posts is to pass along relevant information from the medical community – direct from the source – with some translation into regular English.
I want to keep you informed as best as I can.
Latest Numbers
Total United States cases: 10,442
— Travel-related: 290
— Close contact: 310
— Under investigation: 9,842
Total deaths: 150
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, and US Virgin Islands
(Numbers pulled from other reliable resources) Total United States cases reported by other medical sites:
Johns Hopkins:
Total cases: 13,768
Total deaths: 200
Total recovered: 108
Higher totals may be reported by other news agencies. This information is pulled straight from official government / medical university websites only. The numbers may conflict. If I understand things correctly, the CDC site is pulled from reports they receive by noon while Johns Hopkins pulls in data continuously.
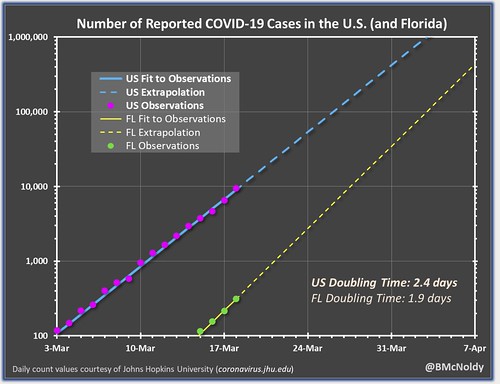
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put that chart together. As it notes, it is pulling numbers from the Johns Hopkins totals. It shows the double-time of cases as about two-and-a-half days. It has not updated with the evening numbers yet, but when it does, I will replace the chart (and deleted this sentence).
Before we get going…
Please know that this is not an exhaustive list of information. I’m trying to pick out some of the bigger notes from the day / past 24 hours. If you are curious about a specific topic related to COVID-19, try to search the blog for more information, I may have discussed it earlier this week or last week.
but so much stuff is happening at once, it is difficult to – not only keep up – distribute all of the information out there.
Slow the spread
According to Johns Hopkins the virus can spread through airborne transmission. Research has shown that tiny droplets remain in the air even after the person with the virus leaves the area. These can remain airborne for up to three hours. This is why it is important to avoid people who are coughing. Even if you are walking 10ft behind them, you may still be at risk for inhaling one of the microscopic airborne droplets. Even hours later.
Those droplets are usually – according to the National Center for Biotechnology Information – under 5 micrometers in size. The Coronavirus itself is about 120 nanometers in size.
So for easy math, let’s say someone sneezes and leaves airborne droplets that at 4 micrometers in size. Those tiny droplets float around – and there could be hundreds – carrying with them about 30 viruses each. And those viruses can start to multiply the second they get into your system.
And because humans don’t have a natural immunity to the infection, each person’s antibodies has to learn how to attack the virus and fight it off. And, due to how the virus multiplies and reproduces itself, that could leave older people more susceptible due to the increased blood sugar (based on research).
Postpone any surgeries
From Johns Hopkins:
The Centers for Medicare and Medicaid Services (CMS) issued guidance that all elective surgeries and procedures, including medical and dental, be postponed nationwide. This recommendation aims to mitigate the burden on health systems due to increasing COVID-19 incidence and make necessary equipment, supplies (including personal protective equipment), and personnel available to treat these patients. Additionally, the guidance notes that dental procedures pose a high risk for transmission due to the close proximity of providers and patients. CMS presents a tiered framework for determining whether procedures should be performed.
From the CDC
The CDC released preliminary numbers for the infections so far. In the report, as of March 16, 4,226 COVID-19 cases had been reported in the United States. That number is now, three days later, 10,442. The report notes that news cases are now popping up at 500 or more cases per day.
Among 2,449 patients with known age, six-percent were aged ≥85, 25-percent were aged 65–84 years, 18-percent each were aged 55–64 years and 45–54 years, and 29-percent were aged 20–44 years (Figure 2). Only five-percent of cases occurred in persons aged 0–19 years.
Among 508 (12-percent) patients known to have been hospitalized, nine-percent were aged ≥85 years, 26-percent were aged 65–84 years, 17-percent were aged 55–64 years, 18-percent were 45–54 years, and 20-percent were aged 20–44 years. Less than one-percent of hospitalizations were among persons aged ≤19 years.
The percentage of persons hospitalized increased with age, from 2%–3% among persons aged ≤9 years, to ≥31% among adults aged ≥85 years.
Let’s unpack that real fast.
That means, from the time of this report, researchers only knew the age of about 60-percent of those infected. Of those 60-percent…
– 146 were older than 85
– 612 were between 65 and 84
– 440 were between 54 and 65
– 440 were between 45 and 54
– 710 were between 20 and 44
– 122 were younger than 19
That means about 46-percent, 1130 people, of those with a known age were in the workforce. If we extrapolate that percentage out to today’s number of 10,442, that means about 4800 people who could be working, are (hopefully) not working because of COVID-19.
In three days, using this extrapolation, the number of working-aged people has increased FOUR fold. That is incredible.
Doing the same calculation with those who were hospitalized gets you 1,255 estimated people hospitalized. And 690 of those were between 20 and 54. That number has doubled in three days.
If it doubles again in three days, that is 2,500. Another three days? 5,000 Another three days? 10,000 people. Hospitalized by this. By the end of next week.
By next Friday, extrapolating out the working-class numbers above, using the same four-fold increase, and 307,200 people will have the virus.
With a two-percent fatality rate of those 307,200 estimated people, 6,144 would die. And those who would die, would within six weeks as the virus took its course..
And while I have discussed the dangers of extrapolation before, and while this is an exaggerated example, this is why social distancing is so important. It will help curb those numbers dramatically if we all do our part.
More from the CDC…
Among 44 cases with known outcome, 15 (34-percent) deaths were reported among adults aged ≥85 years, 20 (46-percent) among adults aged 65–84 years, and nine (20-percent) among adults aged 20–64 years. Case-fatality percentages increased with increasing age, from no deaths reported among persons aged ≤19 years to highest percentages among adults aged ≥85 years.
New clinical trial begins on treatment
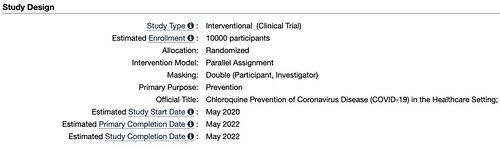
The study, titled, “Chloroquine Prevention of Coronavirus Disease (COVID-19) in the Healthcare Setting” is set to begin in May. Because trials are just starting, I couldn’t find data on any treatments that have already used this drug. The researchers behind the study note:
The study is a double-blind, randomized, placebo-controlled trial that will be conducted in health care settings. After obtaining fully informed consent, the investigator will recruit healthcare workers, or other individuals at significant risk who can be followed reliably for 5 months. 10,000 participants will be recruited and the investigator predict an average of 200 participants per site in 50 sites.
The participant will be randomized to receive either chloroquine or placebo (1:1 randomization). A loading dose of 10mg base/kg, followed by 150 mg daily (250mg chloroquine phosphate salt) which will be taken for 3 months or until they are diagnosed with COVID-19. Subsequent episodes of symptomatic respiratory illness, including symptomatic COVID-19, clinical outcomes, and asymptomatic infection with the virus causing COVID-19 will be recorded during the follow-up period.
But, don’t look for Chloroquine to be widely administered to patients any time soon.
The clinical trial ends in May. Of 2022.
From the Mayo Clinic
The Mayo Clinic shot out a press release today suggesting they have “significantly expanded its capacity to test clinical samples for SARS-CoV-2,” the virus that causes COVID-19. The equipment wen online Tuesday and will test samples from all Mayo Clinics. The new technology can process as many as 4,000 COVID-19 tests daily.
The Mayo Clinic also released another podcast covering the importance of flattening the curve.
And a reminder to keep your workstation clean.
From Harvard Medical
Harvard loaded some quick information about the COVID-19 testing onto its website.
Tests are becoming more widely available and are being processed in commercial labs and academic centers across the country. In the US, the most common test for the COVID-19 virus looks for viral RNA in a sample taken with a swab from a person’s nose or throat. Currently, you can expect the test results within three to four days. Likely the turnaround time for results will be shorter over the next few weeks.
If a test result comes back positive, it is almost certain that the person is infected.
A negative test result is less definite. An infected person could get a so-called “false negative” test result if the swab missed the virus, for example, or because of an inadequacy of the test itself. We also don’t yet know at what point during the course of illness a test becomes positive.
If you experience COVID-like symptoms and get a negative test result, there is no reason to repeat the test unless your symptoms get worse. If your symptoms do worsen, call your doctor or local or state healthcare department for guidance on further testing. You should also self-isolate at home. Wear a mask if you have one when interacting with members of your household. And practice social distancing.
Plus two podcasts / interviews that may be of interest:
The COVID-19 outbreak has caused markets to collapse and worldwide health systems to become overwhelmed. When there’s a global pandemic, it’s nice to hear from the steady, transparent and yes even reassuring voice of experts on the front lines. We spoke to Dr. Ashish K. Jha, faculty director of the Harvard Global Health Institute. Dr. Jha’s recent appearance on the PBS Newshour caused reverberations throughout the federal and state response system. Here’s his update.
Dr. Greg L. Fricchione, Mind Body Medical Institute Professor of Psychiatry at Mass General Hospital and Harvard Medical School and faculty editor for the Harvard Health Publishing special health report Stress Management, places in context the worries we all feel when an infectious disease like the coronavirus COVID-19 comes calling.
What should I do, right now?
I know. It can seem overwhelming with the amount of information and updates flying around. But I think it is best to follow the CDC’s guidance at this point.
— Know where to get your local / state-level information
For Mississippi: https://msdh.ms.gov/msdhsite/_static/14,0,420.html
For Louisiana: http://ldh.la.gov/Coronavirus/
For Alabama: http://www.alabamapublichealth.gov/infectiousdiseases/2019-coronavirus.html
If you live in a state outside of the region, head to google and type in, “dept of health” followed by whatever state you live. Google should take you to that state’s department of health and on the main page, most states have a link to an update on the Coronavirus.
— Know the Symptoms
Look for things like a fever, dry cough, and shortness of breath. But also know when it may become an emergency. It becomes an emergency when you have difficulty breathing, a persistent pain or pressure in the chest, you develop general confusion, and if you develop bluish lips or face.
Also recognize that body aches, weak stomach, nasal congestion, a sore throat, and other symptoms of the regular flu are not the same as the symptoms with Coronavirus.
— Stay home when you are sick
Any kind of sick. If you feel like you may have Coronavirus, call your health care provider’s office in advance of a visit. If you have any sickness, the CDC recommends to limit movement in the community, limit visitors, and practice good social distancing.
— Know if you are at a higher risk
Know what additional measures those at higher risk and who are vulnerable should take. Those at higher risk include older adults (over 60), people who have serious chronic medical conditions (like heart disease, diabetes, lung disease). Some research has indicated that people with asthma may also be included in the higher risk category.
— Take steps to mitigate your infection
The CDC recommends to “Implement steps to prevent illness” by washing high-traffic areas more often, washing hands with soap and water and if someone is sick, to isolate the sick person into a low-traffic area of the home.
— Create a Household Plan
Create a household plan of action in case of illness in the household or disruption of daily activities due to COVID-19 in the community.


Thank you for all your work Nick, it is appreciated.
Nick as a GenX’er carrying a double whammy of heart disease and asthma, thank you for these informative updates. I have been following the Covid progression in Europe as well as here at home and I appreciate the time/effort you have put in to seek out and disseminate factual information for your viewers. Ironically, the song Bridge over Troubled Waters by Simon and Garfunkel popped up on my playlist as I was reading this. Quite fitting to say the least. Take care out there.