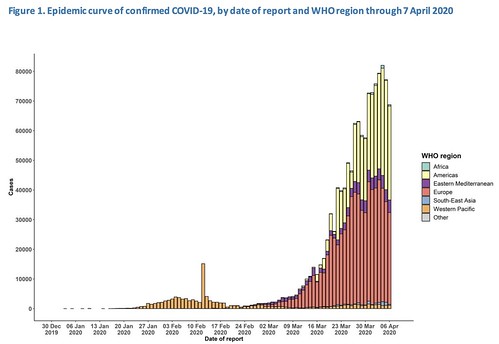
Latest Numbers
WHO Numbers
Total Worldwide Cases: 1,279,722
Total Worldwide Deaths: 72,614
CDC Numbers
Total United States cases: 374,329
— Travel-related: 1,669
— Close contact: 6,847
— Under investigation: 365,813
Total deaths: 12,064
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, the Northern Mariana Islands, and the U.S. Virgin Islands
COVID-19 cases reported by other medical sites:
Johns Hopkins
Total Worldwide Cases: 1,428,428
Total Worldwide Deaths: 82,020
Total Worldwide Recovered: 300,198
Total US cases: 398,185
Total US deaths: 12,844
Total US recovered: 21,849
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put a chart together of the growth. As it notes, it is pulling numbers from the Johns Hopkins totals.
Regional Numbers
| Cases | Tested | Deaths | %-positive | Mortality Rate | |
| MS | 1915 | 20370 | 59 | 9.40% | 3.08% |
| LA | 16284 | 70046 | 582 | 23.25% | 3.57% |
| AL | 2197 | 14765 | 64 | 14.88% | 2.91% |
| TN | 4138 | 52874 | 72 | 7.83% | 1.74% |
| AR | 997 | 13778 | 18 | 7.24% | 1.81% |
| Total | 25531 | 171833 | 795 | 14.86% | 3.11% |
A few states in the region do release the number of hospitalized people due to COVID-19. Those numbers are as follows:
Mississippi: 373
Louisiana: 1,996 (519 on ventilators)
Alabama: 271
Tennessee: 408
Arkansas: Not given
Making Estimates from past research
I talked about research from the Cruise Ships that may be relevant to estimating the number of cases without testing everyone (since that isn’t a feasible option). Plus, this type of estimate would make a good “first guess” at the number of asymptomatic people (the people who don’t feel sick, but are still infected), too.
This type of estimating isn’t perfect. In fact, it is far from it. And it is just an estimate. But based on the past research, it is at least a start.
| Estimated Symptomatic | Estimated Asymptomatic | Estimated total | |
| MS | 2921 | 641 | 3562 |
| LA | 24836 | 5452 | 30288 |
| AL | 3351 | 736 | 4086 |
| TN | 6311 | 1385 | 7697 |
| AR | 1521 | 334 | 1854 |
| Total | 38940 | 8548 | 47488 |
Masks now recommended by the CDC
This isn’t “new” for today, but I think it is worth noting again. Protective masks are now recommended, but not required, when out in public.
According to the CDC:
Cloth face coverings should…
— fit snugly but comfortably against the side of the face
— be secured with ties or ear loops
— include multiple layers of fabric
— allow for breathing without restriction
— be able to be laundered and machine dried without damage or change to shape
CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies), especially in areas of significant community-based transmission.
CDC also advises the use of simple cloth face coverings to slow the spread of the virus and help people who may have the virus and do not know it from transmitting it to others. Cloth face coverings fashioned from household items or made at home from common materials at low cost can be used as an additional, voluntary public health measure.
Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove the mask without assistance.
The cloth face coverings recommended are not surgical masks or N-95 respirators. Those are critical supplies that must continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance.
The CDC says that you should be careful not to touch your eyes, nose, or mouth when removing the mask. And wash your hands immediately after removing.
The CDC has a few quick tips on making your own mask. One way, with no sewing needed, is by cutting an old Tshirt.
There is more information and a tutorial on how to make your own mask here: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html
Hydroxychloroquine and azithromycin
I mentioned on facebook today that a study was published recently showing that a handful of the patients did not recover from the virus when taking Hydroxychloroquine. It turns out the report I was reading what about the study that was in question from yesterday’s post.
This is why I never fault anyone for getting lost in all of this stuff. I keep up with it, and I can’t even keep up at times.
One of the studies titled, “Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial” highlighting Hydroxychloroquine as a remedy for COVID-19 was deemed substandard by the International Society of Antimicrobial Chemotherapy.
This study was cited by the CDC back on March 24:
Due to higher in-vitro activity against SARS-CoV-2 and its wider availability in the United States compared with chloroquine, hydroxychloroquine has been administered to hospitalized COVID-19 patients on an uncontrolled basis in multiple countries, including in the United States. One small study reported that hydroxychloroquine alone or in combination with azithromycin reduced detection of SARS-CoV-2 RNA in upper respiratory tract specimens compared with a non-randomized control group but did not assess clinical benefit [7]. Hydroxychloroquine and azithromycin are associated with QT prolongation and caution is advised when considering these drugs in patients with chronic medical conditions (e.g. renal failure, hepatic disease) or who are receiving medications that might interact to cause arrythmias.
The ISAC pulled the paper (A friendly hat-tip to https://retractionwatch.com/ for the heads up on this one) due to questions about patient safety and inclusion criteria. The original findings from the study’s authors found that: “Despite its small sample size our survey shows that hydroxychloroquine treatment is significantly associated with viral load reduction/disappearance in COVID-19 patients and its effect is reinforced by azithromycin.”
However the ISAC says:
ISAC shares the concerns regarding the above article published recently in the International Journal of Antimicrobial Agents (IJAA). The ISAC Board believes the article does not meet the Society’s expected standard, especially relating to the lack of better explanations of the inclusion criteria and the triage of patients to ensure patient safety.
Despite some suggestions online as to the reliability of the article’s peer review process, the process did adhere to the industry’s peer review rules. Given his role as Editor in Chief of this journal, Jean-Marc Rolain had no involvement in the peer review of the manuscript and has no access to information regarding its peer review. Full responsibility for the manuscript’s peer review process was delegated to an Associate Editor.
Although ISAC recognises it is important to help the scientific community by publishing new data fast, this cannot be at the cost of reducing scientific scrutiny and best practices. Both Editors in Chief of our journals (IJAA and Journal of Global Antimicrobial Resistance) are in full agreement.
What does all of this mean? Yesterday I mentioned that this was a good question. After further reading, though, I tend to think this study is just going to be retracted. Sadly, unlike weather studies, they cannot simply re-create the same environment again. And this was a pretty flawed environment.
It started with 40 patients, but only 36 finished. Six did not. Five by choice, one by death. And the average age of the group that were treated was much different than the one who was not treated. And it was an open-label test, note the “double-blind” test that the medical community generally uses to make sure data isn’t skewed.
So, there were a handful of issues. If the researchers wanted to re-do the study, they would need to find another group of patients and change their procedures. It could be done, but I don’t think the findings from a new study would be published under the same article. They would just prepare and write a new study and paper.
Iceland study inds 50-percent of COVID patients are asymptomatic
I saw this headline today, but could not find any “on paper” evidence to back it up. The article that reported it said that DeCODE’s, a subsidiary of US biotech company Amgen, founder Dr. Kári Stefánsson said that “around 50% of those who tested positive said they were asymptomatic, confirming multiple studies that show that asymptomatic, or mildly symptomatic, people have played an important role in spreading the virus.”
That that’s fine. But, like, where is the proof? The closest thing I could find was a post from Iceland’s government:
A total of 5 564 tests have been performed by the National University hospital of Iceland in Reykjavík, mostly on individuals who were symptomatic or were considered to be likely to have contracted the virus due to proximity to infected individuals or other reasons. Out of these 5,564 tests, 4,879 have been negative and 685 positive.
A total of 6 163 tests have been performed on the general population, individuals who had not been ordered to quarantine and were generally asymptomatic or showed mild symptoms. Out of these 6,163 tests, 6,111 have been negative and 52 positive.
And even if we assume that all 52 “generally asymptomatic or showed mild symptoms” people were fully asymptomatic, that is still not 50-percent of the total people testing positive. Because adding 685 people (who were symptomatic) PLUS the 52 (that we are assuming are asymptomatic), divided in half is not – also – 52.
That’s easy math. Half of 685 + 52 is closer to 368.
The symptomatic vs. asymptomatic ratio that I prefer is the one from the cruise ships (linked above) since that is a fair estimate for a known population where the known population was fully-tested. And tracked.
That showed an asymptomatic percentage around 18-percent. Meaning of the 52 that were “generally asymptomatic or showed mild symptoms” we can assume about 9 or 10 were actually asymptomatic.
That is, until the numbers are published.
Mosquitoes aren’t carries of this virus
The World Health Organization made a quick “MythBuster” about mosquitoes. They mentioned that, to date, there has been “no information nor evidence to suggest that the new coronavirus could be transmitted by mosquitoes.”
Instead, as they remind everyone, it is spread by respiratory droplets from humans. So cover your cough and sneeze.

From Harvard Medical
There has been a lot of buzz in the news about “convalescent plasma” to help people with COVID-19. Harvard took the time to explain what that is, and how it can help those fighting the virus.
When people recover from COVID-19, their blood contains antibodies that their bodies produced to fight the coronavirus and help them get well. Antibodies are found in plasma, a component of blood.
Convalescent plasma — literally plasma from recovered patients — has been used for more than 100 years to treat a variety of illnesses from measles to polio, chickenpox, and SARS. In the current situation, antibody-containing plasma from a recovered patient is given by transfusion to a patient who is suffering from COVID-19. The donor antibodies help the patient fight the illness, possibly shortening the length or reducing the severity of the disease.
Though convalescent plasma has been used for many years, and with varying success, not much is known about how effective it is for treating COVID-19. There have been reports of success from China, but no randomized, controlled studies (the gold standard for research studies) have been done. Experts also don’t yet know the best time during the course of the illness to give plasma.
On March 24th, the FDA began allowing convalescent plasma to be used in patients with serious or immediately life-threatening COVID-19 infections. This treatment is still considered experimental.
From Johns Hopkins
In the daily “Situation Report” Johns Hopkins posted abou a new CDC report. This is for parents, mostly.
The US CDC COVID-19 Response Team published a study of COVID-19 disease presentation and severity in US children. The study, published in the CDC’s Morbidity and Mortality Weekly Report , analyzed clinical data for 149,082 COVID-19 patients in the United States reported between February 12-April 2, including 2,572 pediatric patients.
Pediatric patients represented only 1.7% of those patients. Compared to adult COVID-19 patients, fewer pediatric patients experienced fever, cough, or shortness of breath (73% vs 93%). With respect to disease severity, only 5.7% of pediatric patients were hospitalized, compared to 10% for adult patients. Three deaths were reported among the pediatric patients, but investigation is still ongoing to determine if COVID-19 was the likely cause of death in these patients.
The study also provides analysis of underlying conditions in pediatric patients. Among those with available data (345 cases), 23% had at least 1 underlying health condition, with chronic lung disease (including asthma), heart disease, and compromised immune system being the most commonly reported.
These data support the current understanding that COVID-19 disease tends to be more severe in adults than in children; however, severe disease and death can still occur in pediatric patients.
I read through the study briefly and the one thing I noticed is that any symptom was less likely in children. Across the board. Except one!
Runny nose.
| Sign/Symptom | Number (Percentage) | |
| Kids | Adults | |
| Fever, cough, or shortness of breath† | 213 (73) | 10,167 (93) |
| Fever | 163 (56) | 7,794 (71) |
| Cough | 158 (54) | 8,775 (80) |
| Shortness of breath | 39 (13) | 4,674 (43) |
| Myalgia | 66 (23) | 6,713 (61) |
| Runny nose | 21 (7.2) | 757 (6.9) |
| Sore throat | 71 (24) | 3,795 (35) |
| Headache | 81 (28) | 6,335 (58) |
| Nausea/Vomiting | 31 (11) | 1,746 (16) |
| Abdominal pain | 17 (5.8) | 1,329 (12) |
| Diarrhea | 37 (13) | 3,353 (31) |
Only about half the kids had a fever and about 15-percent had shortness of breath. So, as I reported from a separate study earlier, figuring out if your kids are sick with COVID-19 might be more difficult.
Hang in there
I know we are all getting tired of this. I know because I, too, am getting tired of this. But we have to stick it out and stick together – separately. Social Distancing seems to be helping and the medical community says it is our best defense against this virus.
So keep up the good work friends. We can do this!




Thank you Nick for all the information. I follow it nightly and really appreciate the time and effort that you put into this. You are a blessing.