I’m not a doctor. Still. A lot of people have accused me of trying to be one and encouraged me – sometimes rudely – to “Stay in my lane” or “stick to weather” because I am not a doctor.
But I want to reassure everyone that I am not sharing any personal opinions on any of these posts. Ever. I am not qualified to have an opinion. All I can do is cultivate information from the medical research community and pass it along to you. The goal is to keep you as informed as possible during this pandemic.
Any and all COVID-related advice you read about here is direct from the medical community and not the opinion of a meteorologist. Because, again, I am not qualified to offer an opinion.
The idea of “Superspreaders” proposed
In a few different papers, researchers have started to look at the potential for “superspreaders” of the virus. These are people who carry abnormally high viral loads and end up infecting more people than the average R0 value of 2-to-3.
Examples of a “Superspreader” would be the pastor and his wife in Arkansas that infected more than 20 people and the choir singer in Washington that was tied to infecting more than 50 people.
The disproportionate number of people infected by superspreaders, researchers say, may explain the pattern of how COVID-19 is spreading.
In a recent paper titled, “Do superspreaders generate new superspreaders? A hypothesis to explain the propagation pattern of COVID-19” the idea that superspreaders “include high viral shedding due to poor immunocompetence, underlying diseases or co-infection, or elevated contact rate due to active social behaviour (Bassetti et al., 2005; Lloyd-Smith et al., 2005, McDonald et al., 2004, Shen et al., 2004, Wong et al., 2015).”
The authors wrote:
It appears that SARS-CoV-2 spreads gradually within a region unless a chain reaction of transmission is triggered. Independent superspreading events due to individual variation cannot explain this large-scale heterogeneous pattern of transmission. The occurrence of superspreaders may not be at random and may depend on other superspreaders. It is proposed that infections caused by contact with superspreaders are more likely to result in new superspreaders than those caused by transmission from a less infectious individual. The mechanism by which this would be possible is by exposure to differential viral load. The primary mode of transmission of SARS-CoV-2 appears to be through exposure to respiratory droplets and direct contact with infected individuals and their contaminated environment (Xiao et al., 2017, van Doremalen et al., 2020). Droplets may contain a few or a million viral particles, and this differential load determines how much the environment is contaminated and the infective dose a susceptible person is exposed to.
To unpack that, the authors are suggesting normal spreading doesn’t really account for the random occurrences of drastically increased numbers. Their hypothesis is that people who don’t carry as high a viral load, will not “sneeze out” or “cough out” as many viruses in their droplets that are expelled. And people with a higher viral load will expel a much higher density of viruses.
When people come into contact with a higher density/volume/number of viruses, the hypothesis is that those people are then carriers of a higher viral load themselves.
The authors continue:
Infections resulting from exposure to high loads of virus are expected to be of high intensity, as a large quantity of viral particles initiating replication in synchrony might overwhelm the mechanisms of resistance, and the poor control of viral replication may therefore result in a new potential superspreader.
Under the hypothesis posited here, cases with low-to-moderate intensity of infection would mainly yield new infections of low-to-moderate severity and viral shedding in people who are not in risk groups.
It is a fascinating hypothesis. And one that other researchers are starting to explore. In a separate paper titled, “Clustering and superspreading potential of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections in Hong Kong” the authors found that, “Superspreading events have characterised previous epidemics of severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) infections. Using contact tracing data, we identified and characterized SARS-CoV-2 clusters in Hong Kong. Given a superspreading threshold of 6-8 secondary cases, we identified 5-7 probable superspreading events and evidence of substantial overdispersion in transmissibility, and estimated that 20% of cases were responsible for 80% of local transmission.”
And that is an incredible proposed statistic. Twenty-percent of cases are responsible for 80-percent of the spread.
The knee-jerk response may be to simply find those who are “superspreaders” and make sure they can’t “superspread” anymore… And leave the rest of the world to get back to normal.
On paper, that works. In reality, it may not be that easy.
It has been noted that some high-viral-load-carriers could be asymptomatic people. Meaning they have a high viral load, they are very contagious, they have the capability of spreading it to others, turning them into “superspreaders” and have no idea they are even infected.
This is why the CDC is really encouraging everyone to wear a mask, socially distance and wash your hands.
Numbers continue to rise, but death rate doesn’t

This may not be true for everywhere in the country, but for Mississippi there has been a recent increase in the number of COVID-19 cases, but not an increase in deaths.
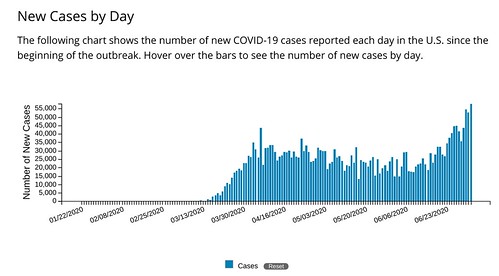
Since June 15th, there has not been a single day with fewer than 350 new cases. Including eight days with more than 600 new cases.
Yet, during that same time the number of deaths per day has average about 10 people. Down from about 12 people a few weeks ago. And 14 a few weeks before than.
And there are a few hypotheses out there, yet to be proven or disproven.
Hypotheses:
1. The virus isn’t as potent as it was
2. The next few weeks will determine the true death rate, due to lag time
The good/bad news is that during the next three weeks, we will find out which hypothesis is most likely to be true. Because the “lag time” hypothesis is just a matter of waiting two or three weeks to find out how many people die from becoming infected during the last week or two.
Which bodily fluids carry the virus
From the CDC:
SARS-CoV-2 RNA has been detected in upper and lower respiratory tract specimens, and SARS-CoV-2 virus has been isolated from upper respiratory tract specimens and bronchoalveolar lavage fluid. SARS-CoV-2 RNA has been detected in blood and stool specimens, and SARS-CoV-2 virus has been isolated in cell culture from the stool of some patients, including a patient with pneumonia 15 days after symptom onset.
The duration of SARS-CoV-2 RNA detection in upper and lower respiratory tract specimens and in extrapulmonary specimens is not yet known but may be several weeks or longer. Duration of several week or longer has been observed in cases of MERS-CoV or SARS-CoV infection.
While viable, infectious SARS-CoV has been isolated from respiratory, blood, urine, and stool specimens, viable, infectious MERS-CoV has only been isolated from respiratory tract specimens. It is not yet known whether other non-respiratory body fluids from an infected person including vomit, urine, breast milk, or semen can contain viable, infectious SARS-CoV-2.


I appreciate you collecting and “unpacking” the data. Keep up the good work!