It was a busy weekend. A lot happened with respect to COVID-19 and the fight to find a vaccine, treatment and a way to slow the spread.
A quick reminder: I’m not a doctor. These posts are not intended to claim any expertise on any medical subject matter. The goal of these posts is to relay, to you, what the medical professionals and official government sources are saying about the pandemic. Always consult your personal doctor with any specific questions you may have about your health and wellness.
A quick note before we get going, too. There seems to be an increase in the number of people skeptical of the heightened concern people have for the increasing number of cases in the United States. Skeptics argue that there are more people here so more cases are natural and no big deal. Or that, because more people are being tested, that is why more positive cases are being found.
Medical professionals that I’ve consulted and papers I’ve read do not think the virus is “spreading faster” as the transmission rate is reasonably well estimated – and concerning enough. But rather, the extra level of concern is the realization of how ubiquitous this all is and the threat that ubiquitousness represents to the vulnerable populations.
The latest statistics
WHO Numbers
Total Worldwide Cases: 693.224
Total Worldwide Deaths: 33,106
CDC Numbers
Total United States cases: 140,904
— Travel-related: 886
— Close contact: 2,151
— Under investigation: 137,667
Total deaths: 2,405
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, and US Virgin Islands
COVID-19 cases reported by other medical sites:
Johns Hopkins
Total Worldwide Cases: 784,716
Total Worldwide Deaths: 37,639
Total Worldwide Recovered: 165,370
Total US cases: 163,807
Total US deaths: 3,008
Total US recovered: 5,846
These numbers differ because they are constantly being updated rather than just a snapshot upgrade in numbers once per day.
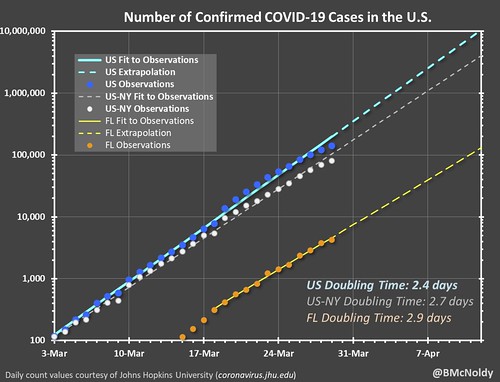
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put a chart together of the growth. As it notes, it is pulling numbers from the Johns Hopkins totals. It shows the double-time of cases as about two-and-a-half days.
Regional Numbers
| Cases | Tested | Deaths | Percent-positive | Mortality Rate | |
| Mississippi | 847 | N/A | 16 | #VALUE! | 1.89% |
| Louisiana | 4025 | 30853 | 185 | 13.05% | 4.60% |
| Alabama | 947 | 6531 | 6 | 14.50% | 0.63% |
| Tennessee | 1834 | 23304 | 13 | 7.87% | 0.71% |
| Arkansas | 508 | 6028 | 7 | 8.43% | 1.38% |
| Total | 8161 | 66716 | 227 | 12.23% | 2.78% |
A few states in the region do release the number of hospitalized people due to COVID-19. Those numbers are as follows:
Mississippi: 195 (+12)
Louisiana: 1,158 (+31)
Alabama: Not given
Tennessee: 148 (+15)
Arkansas: Not given
Making Estimates from past research
I talked about research from the Cruise Ships that may be relevant to estimating the number of cases without testing everyone (since that isn’t a feasible option). Plus, this type of estimate would make a good “first guess” at the number of asymptomatic people (the people who don’t feel sick, but are still infected), too.
This type of estimating isn’t perfect. In fact, it is far from it. And it is just an estimate. But based on the past research, it is at least a start.
| Estimated Symptomatic | Estimated Asymptomatic | Estimated total | |
| Mississippi | 1292 | 284 | 1575 |
| Louisiana | 6139 | 1348 | 7487 |
| Alabama | 1444 | 317 | 1761 |
| Tennessee | 2797 | 614 | 3411 |
| Arkansas | 775 | 170 | 945 |
| Total | 12447 | 2732 | 15179 |
A doctor was reportedly fired for voicing concerns
I don’t normally like to report on other reports. But I was tipped off to this by a friend in the medical industry and it is a bit alarming. Here is the statement from the American Academy of Emergency Medicine:
According to public statements, TeamHealth and PeaceHealth St. Joseph Medical Center have terminated Dr. Ming Lin. If this is so, AAEM condemns TeamHealth and PeaceHealth St. Joseph Medical Center for terminating Dr. Ming Lin an emergency physician who went public with his concerns over the safety of the hospital staff and his patients in this pandemic. It is an essential duty of a physician to advocate for the health of others. Dr. Lin, as a member of the medical staff, is entitled to full due process and a fair hearing from his peers on the medical staff. TeamHealth, a lay corporation owned by the private equity company the Blackstone Group, should not be the employer of Dr. Lin according to the laws of the state of Washington. Their hand in this termination is not only inexcusable but likely impermissible. We call on the WA state Attorney General and the State Board of Medicine to investigate this circumstance.
I don’t know the whole story. And I’m not going to go down the rabbit hole to try and ascertain the complete truth. But if this holds up as true, it would be a very unfortunate event.
There is a Change.org petition to get the doctor reinstated: https://www.change.org/p/team-health-and-peace-health-st-joseph-s-medical-center-rehire-dr-ming-lin?source_location=topic_page. But, as we all know, change.org doesn’t always do much to change the outcome of an event.
On top of that, it explains why a handful of doctors have recently reached out to me to offer extra information… but asked to remain anonymous.
Sit-down interview with Korea’s top Doctor
This is a great, albeit lengthy, video of an interview with Korea’s top doctor, Professor Kim Woo-joo from Korea University Guro Hospital, in the fight against COVID-19. There is a ton of great information in here. It is subtitled, and there are ads, but it is worth your time.
One of the more interesting things that Woo-joo explains is that most people in Korea are wearing KF94 masks. These are similar to the N95 masks. Woo-joo explains that is helping prevent people from contraction the virus from the airborne droplets.
And in the video Woo-joo notes that the main reason the United States isn’t doing that is to save the masks for medical professionals. But, for people who are contractors, weekend-warriors, etc. I suppose if there is an N95 mask laying around, it wouldn’t hurt to throw it on when you are out and about.
Direct from Doctors and Nurses Pt. 3
Most of the Doctors and nurses in this next part are from Oregon or Washington.
Alexander Asai is a Registered Nurse certified in Critical Care. He requested not not identify his hospital(s), but he is a nurse in Washington State. Asai said that his workload has not increased in response to the outbreak. Noting that, if anything, the amount of RNs getting called off has increased. He explained that due to cancellation of elective surgeries and non-emergent patients, the need for people is lower than normal.
“My hospital has taken steps to turn other areas of the hospital, the CRU and PACU, into ancillary ICU units in the event we are in need of the capacity,” Asai said. “Thankfully, capacity is not an issue at this time.”
Things have changed for hospital workflow, though. The hospital has reduced the number of visitors – to help slow the spread. Asai said that people are being re-trained and moved around, in the event of an emergency situation.
“As of last week, everyone who comes into the hospital has their temperature screened,” Asai said. “We are also asked if we have any respiratory symptoms, and if so, we are not allowed to work. The hospital is also providing scrubs for those working on the COVID unit. Additionally, they are re-training RNs with previous ICU experience who work in other units, especially from PACU and CRU, as these units are being underutilized right now anyway.”
Asai mentioned that he takes extra steps to make certain he is always protecting himself, and every next patient.
“I only use disposable stethoscopes with patients suspected or positive with coronavirus,” he said. “Everyone in ICU wipes down their workstation at the start of shift and only uses that one workstation during their shift.”
Asai mentioned his hospital has ordered extra ventilators.
“With the cross-training of RNs I think we will be fine,” he said. “The issue may be related to a shortage of respiratory therapists (RTs) to manage and make precise adjustments to ventilator settings for patients.”
That is an issue that Aleksandra Cherednichenko brought up yesterday in a separate interview.
The other main difference Asai noted was with the use of PPE. The hospital has told the employees that it has “adequate PPE,” but like many hospitals, it is encouraging doctors and nurses to reuse masks and PAPR hoods.
“This is in line with CDC recommendations when hospitals are low on PPE,” Asai said. “I do think the hospital is doing the best they can given the current situation.”
Asai is also taking steps to make sure he slows the spread outside of the hospital. He wears hospital-issued scrubs, leaves his shoes at work, and is “hyper aware” of hand hygiene.
“I also take a shower as soon as I get home,” he said. “I live with 3 roommates, 2 of whom are also RNs at the hospital. We have increased the amount of surface cleaning we do, especially in the kitchen and bathroom. I still do my best to get outside for exercise, but I don’t drive anywhere to do so. I bike or run from my house and maintain social distance of at least 6 feet when passing others on the sidewalk/trails. When I do go to the grocery stores, I try to go late in the day (I work night shift) and avoid groups of people as much as possible”
Asai got onto the topic of the community response and what people can do to help slow the spread based on research. He mentioned that in Korea, researchers found that 2 out of every 10 people didn’t show symptoms, but were still able to pass the virus to the next person.
Asai said that is a problem.
“What they have found is that there is an approximately 20% asymptomatic carrier rate,” he said of the Korean research. “Hence the importance of social distancing. My biggest concern is that people will continue to go about life as normal because they feel fine. The part that is hard to get across is that social isolation isn’t about your health as an individual, it is about the health of the community and the population as a whole. You may be fine, get mild cold-like symptoms, but others who are immunocompromised or have pre-existing conditions are at increased risk of hospitalization, or critical care (mechanical ventilation), or even death.”
Ending on a positive note, when I asked Asai about his biggest concern, he said that if the worst thing that happens to someone during this pandemic is that they are mandated to stay home for a month, or two, then that isn’t so bad in the long run.
“Take the time to binge Netflix, or take online classes, or play with your kids,” he said. “Try to find the good in the situation. We are in this together. Stay home for those of us who cannot. I [will be] ecstatic if this passes, and everyone acts like we overreacted.”
Asai explained: “Because [it meant] we were prepared and took the appropriate precautions”
More from a different doctor
This video was shown to me by a medical professional as a good in-depth look at more details about this disease. This walk-through isn’t G-rated. It is a bit more PG or PG-13. He does occasionally curse.
But fo you adults, it is a very descriptive explanation.
Things you should be doing now
I know this can all seem overwhelming at times. The sheer amount of information being kicked out by every media outlets is like an avalanche.
So, here are some things: Stay home if you can! Gotta work? That’s understandable. Need food? Sure, head to the store. But try to skip any “for fun” activities in public where you would be interacting with others or in a place with multiple other people.
Some CDC’s guidance:
— Know where to get your local / state-level information
For Mississippi: https://msdh.ms.gov/msdhsite/_static/14,0,420.html
For Louisiana: http://ldh.la.gov/Coronavirus/
For Alabama: http://www.alabamapublichealth.gov/infectiousdiseases/2019-coronavirus.html
If you live in a state outside of the region, head to google and type in, “dept of health” followed by whatever state you live. Google should take you to that state’s department of health and on the main page, most states have a link to an update on the Coronavirus.
— Know the Symptoms
Look for things like a fever, dry cough, and shortness of breath. But also know when it may become an emergency. It becomes an emergency when you have difficulty breathing, a persistent pain or pressure in the chest, you develop general confusion, and if you develop bluish lips or face. Also recognize that body aches, weak stomach, nasal congestion, a sore throat, and other symptoms of the regular flu are not the same as the symptoms with Coronavirus.
— Stay home when you are sick
Any kind of sick. If you feel like you may have Coronavirus, call your health care provider’s office in advance of a visit. If you have any sickness, the CDC recommends to limit movement in the community, limit visitors, and practice good social distancing.
— Know if you are at a higher risk
Know what additional measures those at higher risk and who are vulnerable should take. Those at higher risk include older adults (over 60), people who have serious chronic medical conditions (like heart disease, diabetes, lung disease). Some research has indicated that people with asthma may also be included in the higher risk category.
— Take steps to mitigate your infection
The CDC recommends to “Implement steps to prevent illness” by washing high-traffic areas more often, washing hands with soap and water and if someone is sick, to isolate the sick person into a low-traffic area of the home.
— Create a Household Plan
Create a household plan of action in case of illness in the household or disruption of daily activities due to COVID-19 in the community.